This week the ramblings from red shift looks at a disease which used to be a very common occurrence for me in London, often seen once or twice a week, but while not as common here, I do seem to be coming across more patients in crisis than I used to.
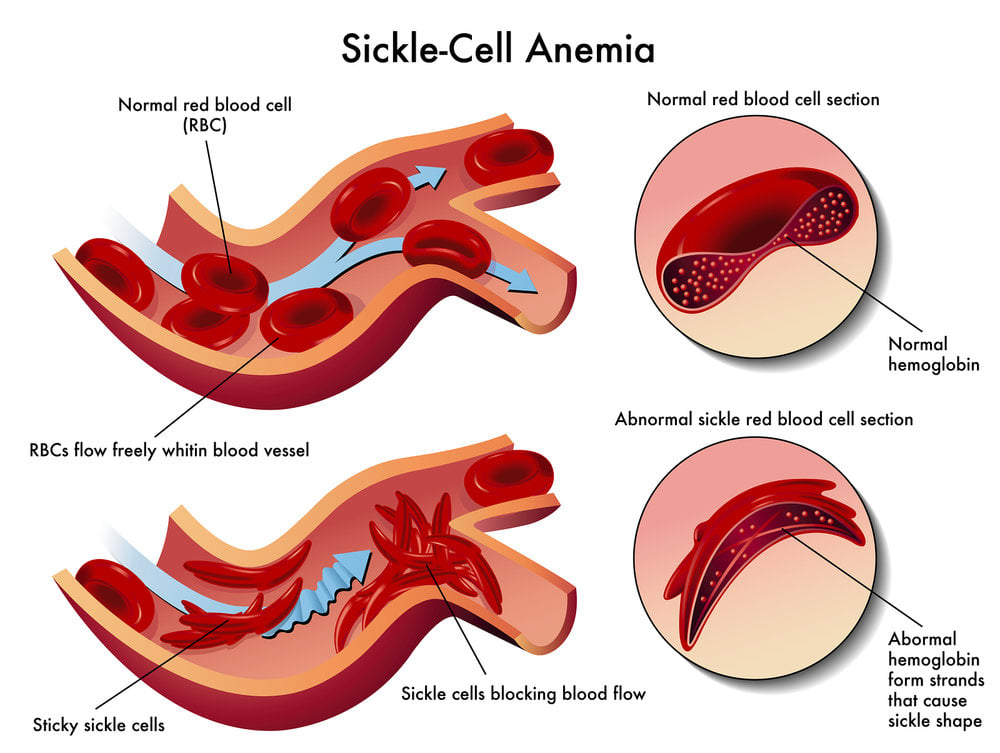
Sickle cell disease is a hereditary condition affecting the haemoglobin contained within red blood cells. These red cells are prone to assuming a permanently sickle shape when exposed to a variety of factors including hypoxia, cold or dehydration – referred to a crisis. These cells are prone to mechanical damage, hence haemolytic anaemia which can lead to occlusion of the microvasculature resulting in tissue hypoxia, pain and organ damage.
These are high risk patients who normally present with normal vital signs but can rapidly deteriorate.
There are different types of sickle cell disease mainly found in people of African or Afro-Caribbean origin, but these can also affect people of Mediterranean, Middle Eastern and Asian origin.

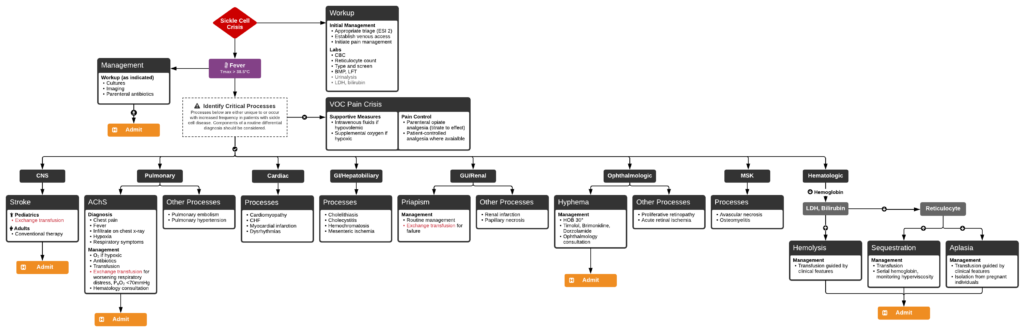
For further reading please visit the links below, the first describes Perth Children’s Hospital’s Sickle Cell ED pathway while the second includes a podcast with relevant reading.

